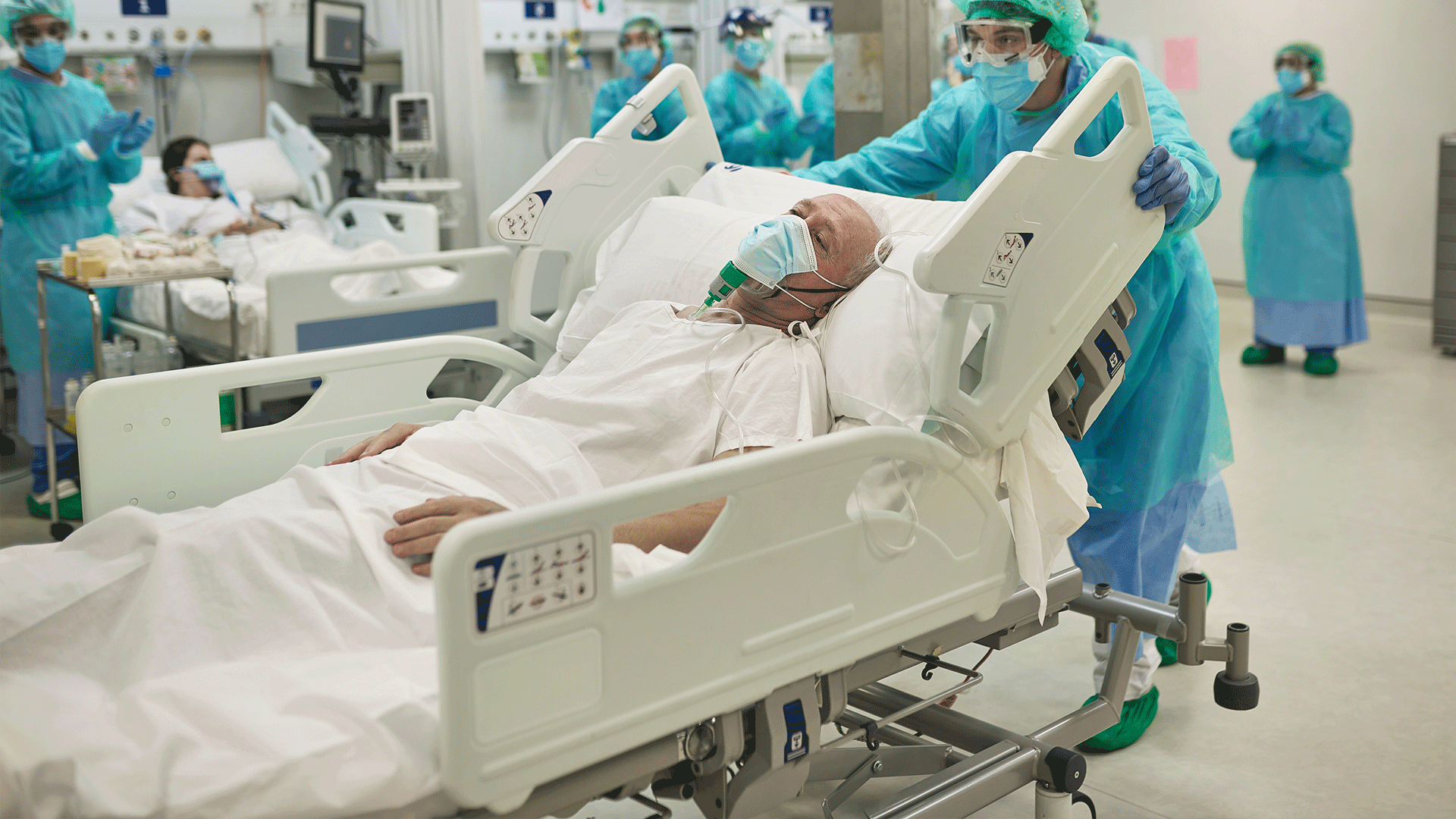
Keep Yourself and Your Family Safe
How to protect yourself — including proper use of PPE — and tips for how to protect your family when you return home after your shift.
The American Nurses Association (ANA) supports all nurses responding to COVID-19, caring for infected individuals and impacted communities, and preventing the spread of the coronavirus within their health care facilities, communities, and families.
How to protect Yourself from COVID-19
Everyday measures to protect yourself from the virus include getting an updated vaccination, frequent hand hygiene, and wearing a face mask in areas of high Covid-19 transmission. When making decisions about prevention strategies and behaviors, you should consider the level of COVID hospitalizations in your area. If you are wearing a mask, experts recommend you upgrade your mask to a high filtration respirator if you want optimal protection. If you think you have been exposed to Covid-19, remember to test soon, and treat early! If you test positive for COVID-19 and have one or more health conditions that increase your risk of becoming very sick, treatment may be available. Contact a health professional right away after a positive test to determine if you may be eligible, even if your symptoms are mild right now. Depending on where you live, there may be a COVID-19 Test-To-Treat location near you. Don’t delay, treatment must be started within the first few days to be effective.
To find a vaccination site near you, visit vaccines.gov.
If you are health care personnel:
- Adhere to the standards for donning and doffing PPE when caring for COVID-19 patients.
- Avoid touching your N95 respirator, facemask, eye goggles, and face shield if wearing during extended use.
- Wash your hands before donning all PPE. When doffing PPE, wash your hands before doffing your goggles, N95 respirator, and face shield, and again after all PPE is doffed.
- Wash your hands frequently with soap and warm water.
- Doff PPE before breaking for meals and taking trips to the restroom.
- Practice hand hygiene before and after going to the restroom and before eating.
- Eat meals in non-clinical areas.
- Disinfect your cell phone frequently, place your cellphone in a clear sealable bag that serves as a barrier, discard of the bag before going home, disinfect your cell phone before entering your home.
- Change your scrubs and shoes if possible before returning home.
N95 Respirator Fit Testing
Fit testing is still required by OSHA. Fit testing ensures the N95 respirator forms a seal around the mouth and nose. If you have not been fit tested for an N95 respirator, your organization or infection control department must provide “just-in-time” fit testing to ensure the N95 respirator is worn properly. Contact your facility’s occupational health department or infection control personnel for your organization’s fit testing requirements.
On June 21, 2021, the U.S. Department of Labor's OSHA issued an Emergency Temporary Standard (ETS) to protect healthcare workers from contracting the Coronavirus Covid-19. This ETS established new requirements for settings where employees provide health care or health support services, including hospitals, skilled nursing homes and home health. On December 27, 2021, OSHA withdrew the non-recordkeeping portions of the healthcare ETS. The COVID-19 log and reporting provisions, 29 CFR 1910.502(q)(2)(ii), (q)(3)(ii)-(iv), and (r), remain in effect. To find out more, see the OSHA Covid-19 ETS Webpage.
Reuse and Decontamination of N95 Respirators
The American Nurses Association continues to advocate aggressively for access to new unused PPE to ensure the ultimate protection of HCP when caring for COVID-19 patients. Read our full statement on the use of decontamination systems here.
As of May 27, 2021, The Food and Drug Administration (FDA) recommends health care personnel and facilities transition away from crisis capacity conservation strategies such as decontaminating disposable respirators for reuse, and the use of non-NIOSH approved disposable respirators such a KN95s. It is recommended that health care facilities increase inventory of available NIOSH-approved respirators including N95s, Elastomeric respirators, including elastomeric respirators without an exhalation valve that can be used in operating rooms, and Powered air-purifying respirators (PAPRs).
The Use of Cloth Masks
Within the health care setting, ANA maintains that all personnel have access to the highest level of respiratory protection to minimize exposure risk to COVID-19. This includes the use of the N95 respirator (or medical facemask with face shield if the N95 respirator is unavailable), face shield, or goggles for eye protection, gown, and gloves. A cloth mask alone does not provide enough respiratory protection from COVID-19 within a medical setting.
Recommendations for the use of cloth masks by the public have changed. Experts now recommend if you are wearing a mask, you upgrade your mask to a high filtration respirator if you want optimal protection. Those who are fully vaccinated may resume many of the activities that you did prior to the pandemic. When making decisions about prevention strategies and behaviors, you should consider the level of COVID hospitalizations in your area. Layering preventive measures such as vaccination, getting a booster, the use of a mask if needed in conjunction with frequent hand washing, and staying home when sick all help to reduce the spread of COVID-19. If you test positive for COVID-19 and have one or more health conditions that increase your risk of becoming very sick, treatment may be available.
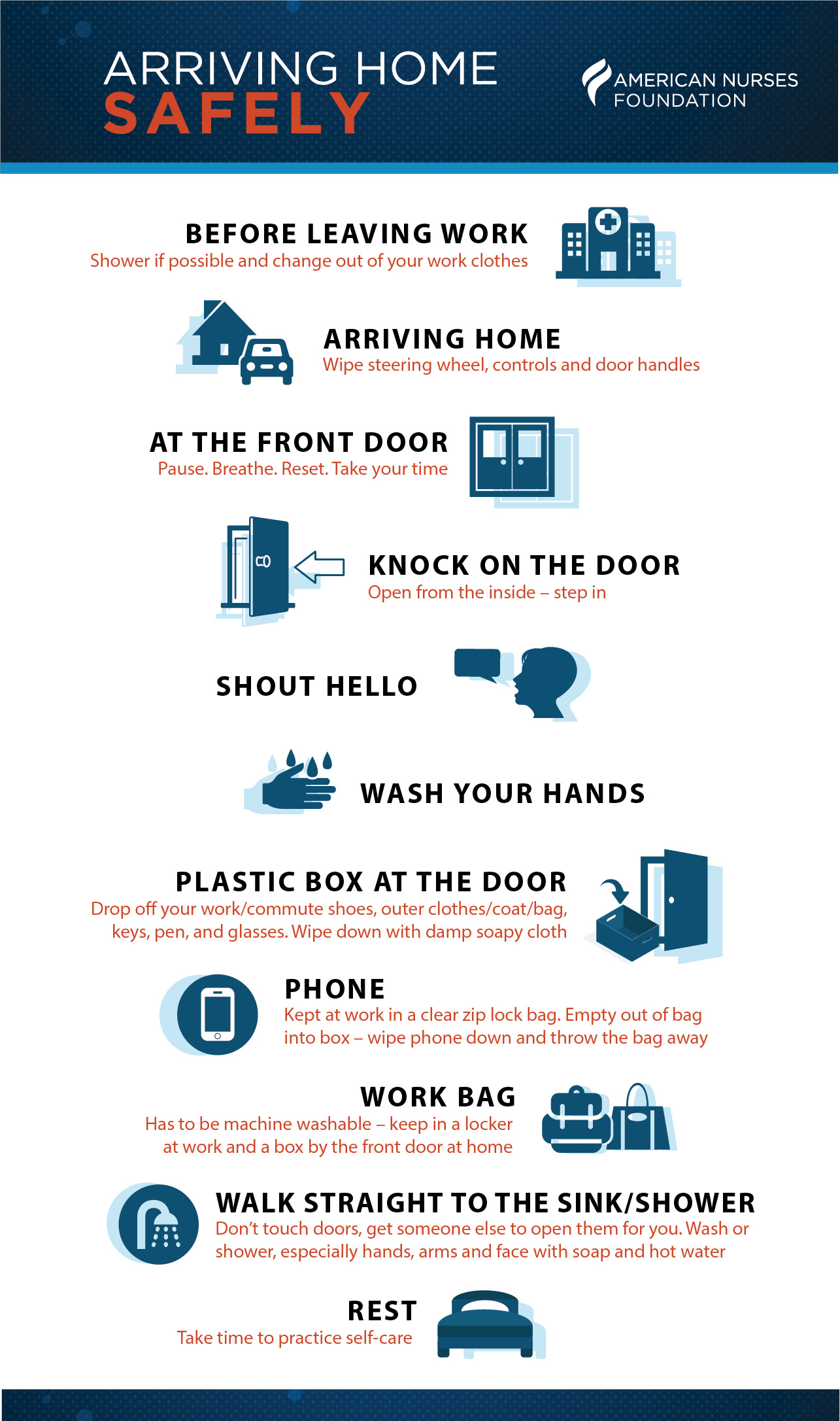
Download Arriving Home Safely Infographic
How to Keep Your Family Safe When You go Home After Your Shift
COVID-19 is primarily spread through respiratory droplets from coughs and sneezes and droplets exhaled when talking that land in the mouth, nose, or eyes of someone in close contact. The virus is also contracted by touching the face, eyes, nose, or mouth with your hands that may have the virus on them. Therefore, cleaning hands and wiping down frequently touched objects, such as a cell phone or tablet, that are commonly transported between home and work is an important step to take prior to returning home. The U.S. Environmental Protection Agency (EPA) has developed a list of products suitable for use against COVID-19.
Additional tips include:
- Remove scrubs and shoes worn while providing care before entry into the home. If possible, wear hospital provided scrubs or carry a change of clothes to work including shoes.
- Remove shoes before entering into the home.
- Keep scrubs contained in a disposable bag, wash in hot water with detergent separately from other laundry items. Dispose of the bag in a lined trashcan once emptied into the washer. Wash your hands.
- Disinfect your cellphone frequently while on the unit and again just before leaving. Consider storing your cellphone in a clear sealable bag as a barrier.
- Leave high touch objects that are not essential for home on your unit, such as pens and clipboards used during your shift, disinfect frequently during the course of your shift.
- If using a personal stethoscope, leave on the unit in a locker, and disinfect before and after use with every patient.
- Wash hands with soap and water upon leaving the unit and again upon entry into the home.
It's also important that your family members understand what COVID-19 is, the symptoms, and the importance of preventative measures such as vaccination, mask wearing and hand hygiene. Encourage your family members to get vaccinated, and get their booster if they are medically eligible.
Guidelines have changed during the course of the pandemic. Those who are fully vaccinated may resume many activities they did prior to the pandemic. However, for the best protection against new and emerging SARS CoV-2 variants, and to prevent possibly spreading it to others, wear a mask indoors in public if you are in an area with a high level of COVID hospitalizations.
Regardless of the level of transmission in your area, if you have a weakened immune system, or are at increased risk for severe disease, wearing a mask provides additional protection. Experts now recommend you upgrade your mask to a high filtration respirator if you want optimal protection. You must also continue to wear a mask where required by laws, rules, regulations, or local guidance.
Reassignment of Health Care Workers Within a Vulnerable Population
Individuals over the age of 65 and with chronic underlying medical conditions are at increased risk of severe morbidity and mortality as a result of COVID-19. If you fall within this category, have a conversation with your employer about redeployment to support telehealth services, transfer to units without COVID-19 patients, or assignment to non-COVID-19 patients needing care. It is also crucial to have access to the appropriate PPE to minimize the risk of exposure.
What to Do If You Are Pregnant
A statement released by the Association of Women’s Health Obstetric and Neonatal Nursing (AWHONN) upholds “Normal physiologic and immunologic changes of pregnancy increase the pregnant woman’s susceptibility to infections. However, data specific to COVID-19 is limited. Pregnant women, their fetuses, and newborns may be at an increased risk for morbidity and mortality if COVID-19 is contracted during pregnancy.” In accordance with recommendations supported by AWHONN, ANA supports the CDC’s recommendation that health care facilities should consider limiting the exposure of pregnant health care personnel to patients with confirmed or suspected COVID-19 during high-risk procedures especially those with increased risk of aerosolization. If you are pregnant and are health care personnel, it is important to continue your routine prenatal care and inform your prenatal care clinician of your exposure risk at work along with any symptoms (including fever, cough, or difficulty breathing) associated with COVID-19. The Society for Maternal-Fetal Medicine (SMFM) and other pregnancy experts recommend that pregnant and lactating people be vaccinated against COVID-19. To read more about the studies confirming safety and efficacy of mRNA COVID-19 vaccines in pregnant and lactating persons, click here.
Recommendations for Breastfeeding Mothers
Research on the risk of pregnant women and breastfeeding mothers associated with COVID-19 continues. The following guidelines are outlined by the CDC for breastfeeding mothers for the protection and prevention of spreading COVID-19 to their infants:
- Breast milk provides protection against many illnesses and is the best source of nutrition for most infants.
- You, along with your family and health care providers, should decide whether and how to start or continue breastfeeding.
- In limited studies, COVID-19 has not been detected in breast milk; however, we do not know for sure whether mothers with COVID-19 can spread the virus via breast milk.
- If you are sick and choose to direct breastfeed:
- Wear a facemask and wash your hands before each feeding.
- If you are sick and choose to express breast milk:
- Express breast milk to establish and maintain milk supply.
- A dedicated breast pump should be provided.
- Wash hands before touching any pump or bottle parts and before expressing breast milk.
- Follow recommendations for proper pump cleaning after each use, cleaning all parts that come into contact with breast milk.
- If possible, consider having someone who is well, feed the expressed breast milk to the infant.
For additional resources on breastfeeding and pregnancy visit the CDC’s Guidance on Pregnancy and Breastfeeding.
Guidance for Protection When Working in Home Health and Home Hospice Care Settings
- Connect with your patient or patient’s family in advance by telephone, text monitoring system, or video conference prior to home visits for temperature and symptom monitoring.
- If you must visit the home and the patient is suspected or confirmed to have COVID-19, wear the following PPE: Gown, gloves, eye protection (goggles or face shield), N95 filtering facepiece, or respirator (or medical facemask if not available). Always perform hand hygiene before donning PPE and after doffing PPE.
- Don and doff PPE outside of the home, dispose of PPE outside the home in a lined trash receptacle, do not travel with used PPE.
- The Centers for Medicare and Medicaid Services provides guidelines for home health care personnel along with detailed guidelines for home hospice care personnel.
Additional Information on Personal Protective Equipment (PPE)
Following the correct sequence of donning and doffing PPE is essential in the prevention of self-inoculation of COVID-19. Below are several links to review the proper sequence along with vital information related to respirator use.
- Use Personal Protective Equipment (PPE) When Caring for Patients with Confirmed or Suspected COVID-19
- Three Key Factors Required for a Respirator to be Effective
- Important Steps for Using NIOSH-Approved N95 Filtering Facepiece Respirators
Information Related to Covid-19 Safety in Schools and Resources for School Nurses
Find more information related to Covid-19 safety in schools, and resources for School Nurses on our Information for School Nurses on Preparedness Planning page, and the National Association of School Nurses Covid-19 Reference page.
Additional Information on Infection Control
For additional information on infection control measures to take within your facility, visit: the Infection Control and Prevention of our site. You can also learn more about infection control, and find training modules for your staff through ANA’s Project Firstline.