Clinical Information
The American Nurses Association supports your ongoing efforts centered on education, prevention, and treatment to mitigate the spread of SARS CoV-2. Continue reading to learn more about the basics of SARS CoV-2 and its associated illness, COVID-19, and find an overview of preparedness and infection control measures.
What is Coronavirus Disease (COVID-19)?
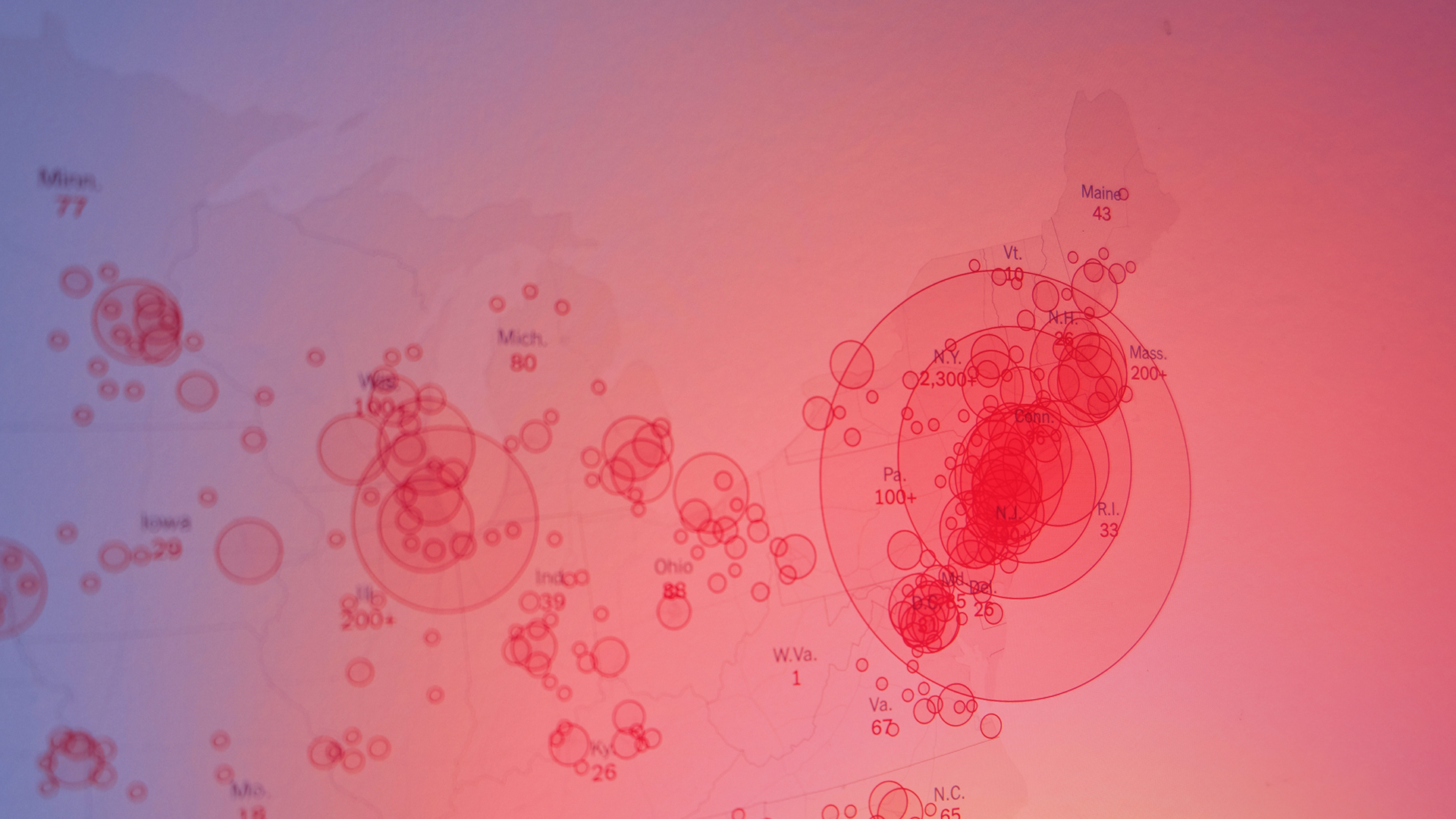
Coronavirus Disease (COVID-19) is the illness that is caused by the coronavirus SARS CoV-2 that was first identified in December 2019 in Wuhan, China. In February 2020, the World Health Organization (WHO) formally named it COVID-19. CO stands for corona, VI for virus, and D for disease. We do know that SARS CoV-2 easily spreads from person to person via respiratory droplets produced from coughs, sneezes, and even while speaking. When a person is within six feet of someone with SARS CoV-2, these droplets may land in the eyes, mouths or noses of individuals, or be breathed into the mouth or nose. It is also possible to contract SARS CoV-2 if the virus is on your hands by touching your eyes, nose, or mouth. SARS CoV-2 can spread in the absence of symptoms.
Click here to learn more about the association between SARS CoV-2 and COVID-19 from Project Firstline.
According to the CDC, symptoms may appear 2-14 days after exposure to the virus. Although, it is also possible for people to have no symptoms. People with these symptoms or combinations of symptoms may have COVID-19:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrhea
Preparedness, Early Identification, and Notification
All nurses and the health care team must receive the highest level of protection to provide care for the individuals and communities in which they serve. It is essential to develop and educate ALL staff on preparedness plans that provide infection control procedures and protocols used within the health care facility for the early identification, containment, and care of patients with symptoms associated with COVID-19 to prevent spread within the facility.
- Obtain updated inventory of all resources needed for response. This includes staffing resources, space, equipment, and PPE.
- Develop inpatient, ambulatory, and home care policies and procedures that are in line with current CDC guidelines for COVID-19
- Provide training to all personnel on screening, isolation and transport procedures
- Provide updated training and guidelines on the use of PPE and infection control measures to prevent the spread within the facility and amongst patients and staff
- Display clear signage with instructions for access and use of PPE
- Ensure consistent use of proper hand hygiene, standard precautions, contact precautions, and airborne precautions, along with the proper use of a National Institute for Occupational Safety and Health (NIOSH)-Approved N-95 respirator or higher (refer to Infection Control and Prevention Section)
- Clearly display signage for patients that lists symptoms and instructions to wear a face mask before entering the health care facility
- To address asymptomatic and pre-symptomatic transmission, update the policy to require everyone (e.g., healthcare personnel, patients, visitors) entering a healthcare facility wear a face mask, regardless of symptoms. This helps prevent transmission from infected individuals who may or may not have symptoms of COVID-19.
- Cloth face coverings are not considered PPE and do not replace the use of PPE for health care personnel. All staff must have access to the appropriate PPE to safely provide care.
- Create a designated point of entry for all patients
- Eliminate visiting hours to protect hospitalized patients from further exposure
- Incorporate assessment questions to document a detailed exposure history
- Identify, in advance, rooms designated, for quarantine and screening
- Plan for patient surge. Cohort patients with respiratory symptoms during triage. Identify a designated unit or wing to cohort patients with confirmed positive COVID-19 tests
- Outline staffing protocols to facilitate care of patients with COVID-19 to minimize patient-to-patient and patient to health care worker transmission. Learn more about staffing and crisis standards of care here.
- Develop a telephone triage protocol for patients to access from home to minimize community-based transmission
- Maintain and communication with the local and state department for updated guidelines and to best assist with contact tracing measures.
OSHA COVID-19 Emergency Temporary Standard
On June 27, 2021, the U.S. Department of Labor's OSHA issued an Emergency Temporary Standard (ETS) to protect healthcare workers from contracting the Coronavirus Covid-19. This ETS established new requirements for settings where employees provide health care or health support services, including hospitals, skilled nursing homes and home health. On December 27, 2021, OSHA withdrew the non-recordkeeping portions of the healthcare ETS. The COVID-19 log and reporting provisions, 29 CFR 1910.502(q)(2)(ii), (q)(3)(ii)-(iv), and (r), remain in effect. To find out more, see the OSHA Covid-19 ETS Webpage.
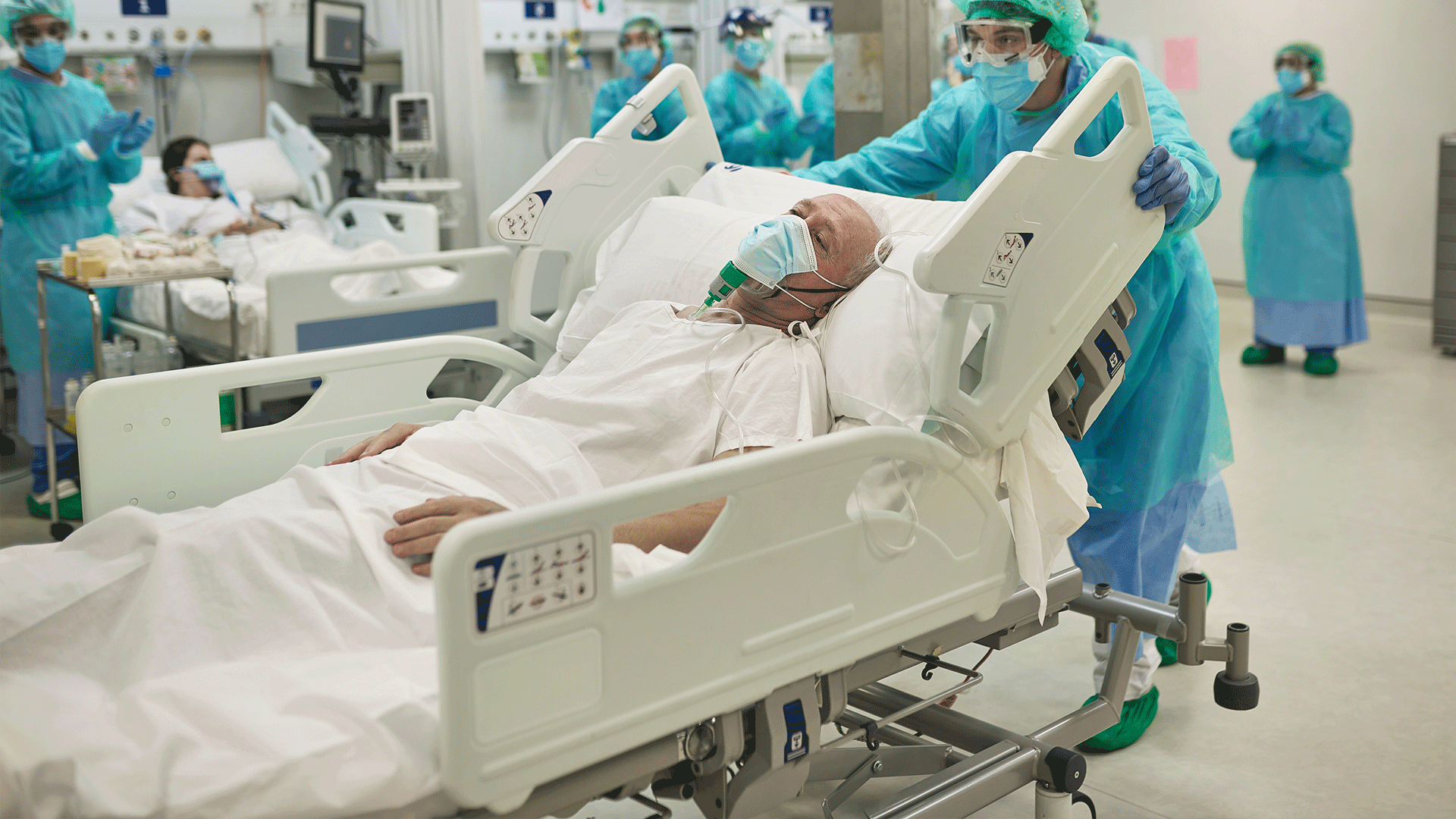
Isolation and Hospitalization
The CDC recommends several steps to identify and care for persons with suspected or confirmed COVID-19.
- Have masks available for patients to don before entering the health care facility
- Once identified, place a patient in a private room with the door closed for assessment. Limit the number of staff entering the room. All staff entering the room must don a N95 respirator, gown, gloves, face shield or goggles for eye protection
- Health care personnel entering the room should use standard precautions, contact precautions, droplet precautions, airborne precautions, and eye protection (goggles or a face shield)
- Have guidelines for the proper use of PPE displayed throughout the health care facility.
- Notify your infection control personnel and the local and state health department of suspected and confirmed positive cases to assist with contact tracing.
See also: the CDC Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic webpage
Treatment Options for Covid-19 Infection
Remember to test soon and treat early! If you test positive for COVID-19 and have one or more health conditions that increase your risk of becoming very sick, treatment may be available. Contact a health professional right away after a positive test to determine if you may be eligible, even if your symptoms are mild right now. Depending on where you live, there may be a COVID-19 Test-To-Treat location near you. Don’t delay, treatment must be started within the first few days to be effective.
Here are links where you can learn more about the current available treatment options (at-home and in-hospital):
• U.S. Department of Health and Human Services (HHS) Possible Treatment Options for COVID-19 website
• Center for Disease Control and Prevention (CDC) Clinical Care Quick Reference for COVID-19 website
• U.S. Health & Human Services (HHS) COVID-19 Public Therapeutic Locator website
Post-Acute Sequelae of COVID-19 (PASC), Long COVID and Post-COVID Conditions
Post-acute sequelae of COVID-19 (PASC), commonly referred to as Long COVID, is a condition marked by persistent COVID-19 symptoms (or the onset of new symptoms) following recovery from acute COVID-19. It is characterized by new, continuing, or recurring respiratory, neurological, psychological, and cardiac problems occurring four or more weeks after initial infection. PASC can affect anyone, even those who had asymptomatic or mild COVID-19 infection. If you or a family member is experiencing prolonged symptoms associated with COVID-19, contact your healthcare provider.
Here is additional information:
- CDC webpage on Long COVID or Post-COVID Conditions
- Yale Medicine - Long COVID (Post-Acute Sequelae of SARS CoV-2 infection, PASC) Fact Sheet
- Johns Hopkins Medicine webpage on COVID ‘Long Haulers’: Long-Term Effects of COVID-19
- CDC webpage Caring for Patients with Post-COVID Conditions
- NIH RECOVER: Researching COVID to Enhance Recovery
- ANA Post-Acute Sequelae of COVID-19 (PASC), Long COVID and Post-COVID Conditions FAQs